- Fast results
- 4,000+ locations
- 4.8 star rating
Need Help? (888) GET LABS


The information in this article is not intended to replace professional medical advice, diagnosis, or treatment. Instead, consult your physician or any licensed healthcare providers if you have medical questions to get personalized answers.
Magnesium is a crucial mineral that contributes to multiple physiological activities in the body. For one, it is a cofactor in over 300 enzymes involved in energy production, muscle functions, bone health, and more. Thus, it is vital to keep your magnesium levels within the optimum range of 1.7 to 2.2 mg/dL.
While knowing the symptoms of magnesium deficiency or surplus can help direct diagnosis, lab tests remain the most prominent way to check for normal magnesium levels. Here are the key steps in determining your serum magnesium.
If you experience unusual symptoms, you’ll likely visit a doctor or undergo a medical test. Therefore, it’s imperative to be familiar with the symptoms of low or high magnesium levels.
Although it’s also likely that some of these symptoms may mimic those of other disorders, at the very least, your doctor can obtain crucial information on general abnormalities in your body. Read on to find out what these symptoms are.
Hypomagnesia is the clinical term for low magnesium levels. Symptoms of this condition vary depending on severity.
For example, mild hypomagnesemia involves the following:
Severe hypomagnesemia is associated with the following symptoms:
Chronic hypomagnesemia(1) requires immediate medical attention. It warrants an emergency trip to the hospital and should be treated immediately.
Hypermagnesemia on its own is actually rare. However, if you have kidney disease, it’s highly possible to also have high magnesium levels because of the impaired ability of the kidneys to filter excess magnesium.
Mild hypermagnesemia often doesn’t show symptoms. However, moderate hypermagnesemia can be characterized by the following:
On the other hand, severe hypermagnesemia can lead to these symptoms:
Symptoms of hypomagnesemia or hypermagnesemia can help direct the diagnosis, but in most cases, they are insufficient. A medical lab test is necessary to confirm the abnormalities in magnesium levels.
A magnesium blood test measures serum magnesium circulating freely. Naturally, a blood sample must be drawn by a licensed medical technician and analyzed in the laboratory.
The normal magnesium level in the blood test result should fall within the range of 1.7 to 2.2 mg/dL. Below the lower threshold, it could signal hypomagnesemia. While over 2.2 mg/dL may indicate hypermagnesemia. Your doctor will check the results and evaluate your symptoms and other information to come up with an accurate diagnosis.
The magnesium RBC test is similar to the standard blood test but is more specific to determining magnesium at the cellular level. It measures stored magnesium in the red blood cells, making it the most accurate lab test on the list.
The normal test result value for the magnesium RBC test is 4.2 to 6.8 mg/dL.
With this test, you’ll need to supply a urine sample so the medical technician can measure magnesium levels expelled by the kidney. There are two types of magnesium urine tests: 24-hour and random tests.
The 24-hour magnesium urine test requires you to collect all your urine within 24 hours. This provides a better picture of your magnesium levels and kidney function. Meanwhile, the random urine test only requires one sample collected anytime during the day.
The normal magnesium level for this test is 24 to 120 mg/day.
Most lab results for magnesium blood and urine tests indicate a reference range for normal levels. The document also outright mentions the abnormality, whether magnesium levels are too high or low.
However, it is discouraged to interpret the test results as they are, especially since many issues involving magnesium levels are related to other health conditions that can be more severe. Consider a telehealth consultation if you want a safe yet remote appointment with a healthcare provider.
Certain health conditions influence normal magnesium levels. In this case, addressing the disease can help correct the deficiency or surplus of the mineral. However, you can help speed up the effectiveness of the treatment by adjusting your diet and making several lifestyle choices.

Supplementation is a likely treatment if you have low magnesium levels, as seen in your urine or blood test. However, if the condition is a direct consequence of another medical problem, dealing with the root cause can also become an offshoot treatment for hypomagnesemia.
For example, if you have osteoporosis, hypertension, or diabetes(2), you’ll also likely have low magnesium. Managing these disorders can normalize magnesium levels.
Nonetheless, consider the following actions to supplement treatment.
Soaking in Epsom salt baths has also been recommended by several experts, as it is believed that magnesium can be absorbed by the skin. However, studies with clinical trials(5) to prove the effectiveness of this method are limited and inconclusive.
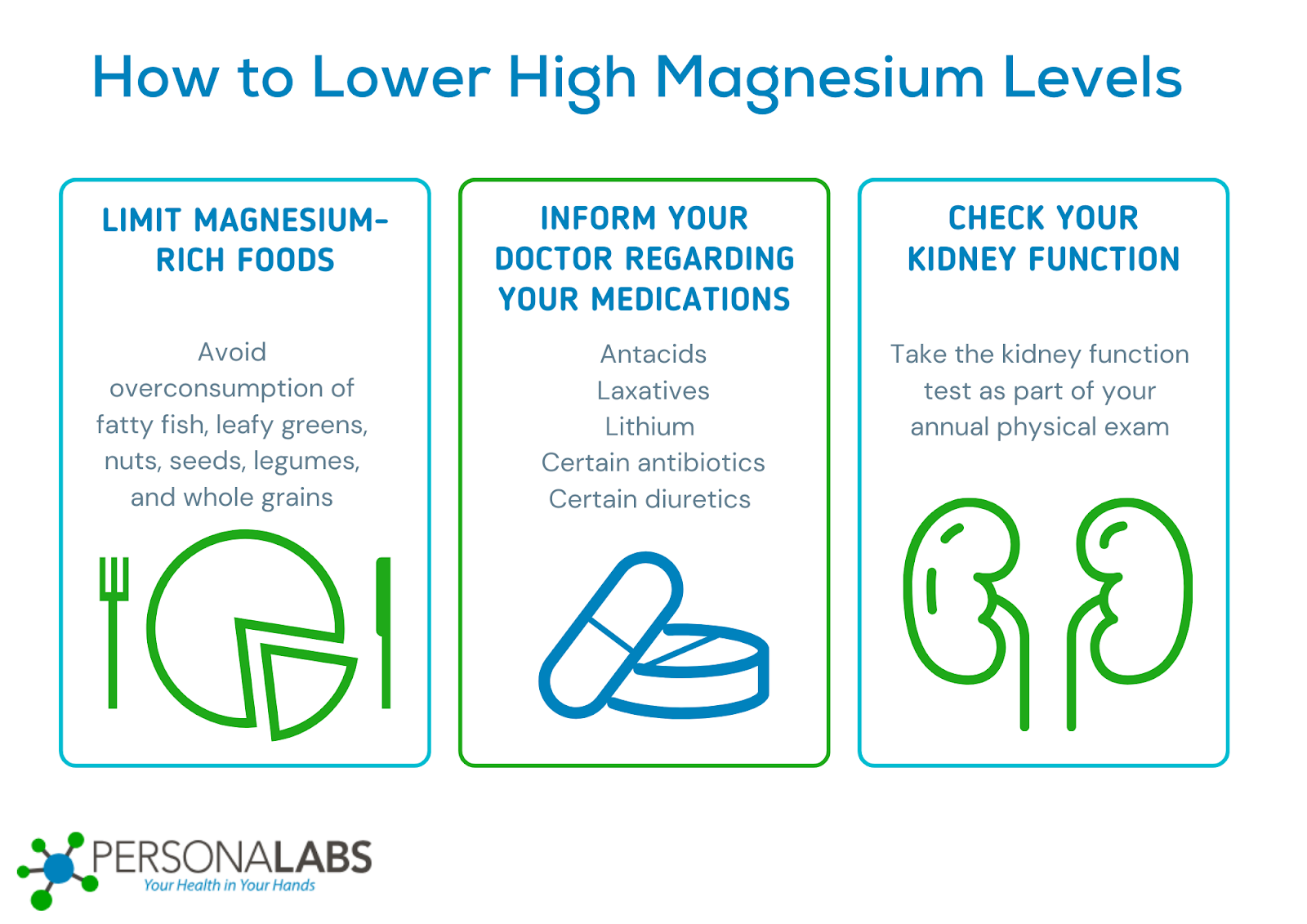
Elevated magnesium can lead to complications involving muscle strength and blood flow, so it shouldn’t be taken for granted. In addition to addressing the underlying condition, you can also take the following actions to bring down high magnesium levels naturally.
Before you start cutting out foods high in magnesium, talk to your doctor first. Without proper planning, you might lose too much magnesium, leading to other health consequences. More importantly, avoid self-diagnosing. Follow the test and treatment your doctor recommends.
Generally, taking magnesium supplements daily is okay and doesn’t harm you. However, your magnesium intake should be within the recommended amount. The dietary allowance for magnesium for adult men is 400-420 mg a day, while women must maintain their intake at 310-320 mg. Consult your doctor for a specific recommendation. Otherwise, you’ll risk developing hypermagnesemia.
As essential as magnesium is to the body, supplementation is discouraged under certain conditions. Some individuals, including those with kidney disease and heart problems, are prohibited from taking magnesium supplements or food sources rich in this mineral due to medical issues. Impaired kidney function can cause magnesium buildup in the blood, which could lead to a slow heart rate.
Likewise, those who are about to undergo surgery must limit their magnesium intake and those taking certain medications, like biphosphonates and diuretics.
If your magnesium level is below 1.25 mg/dL, it is considered severe or critical. You might experience cramps and muscle weakness, along with numbness, irregular heartbeats, seizures, and confusion.
With this number, it’s crucial to seek immediate medical conditions to prevent life-threatening consequences, such as heart and respiratory failure. Critically low magnesium levels can also lead to death.
Like any other must-have nutrients, keeping magnesium at a normal level is crucial. Otherwise, it could disrupt physiological functions and escalate into severe medical problems. To monitor your magnesium levels, be sensitive to symptoms related to hypomagnesemia and hypermagnesemia. Consult your doctor and take the recommended magnesium lab test.
1 Van Laecke S, Nagler EV, Verbeke F, Van Biesen W, Vanholder R. Hypomagnesemia and the risk of death and GFR decline in chronic kidney disease. Am J Med. 2013 Sep;126(9):825-31. doi: 10.1016/j.amjmed.2013.02.036. Epub 2013 Jul 24. PMID: 23891286.
2 Swaminathan R. Magnesium metabolism and its disorders. Clin Biochem Rev. 2003 May;24(2):47-66. PMID: 18568054; PMCID: PMC1855626.
3 Arab A, Rafie N, Amani R, Shirani F. The Role of Magnesium in Sleep Health: a Systematic Review of Available Literature. Biol Trace Elem Res. 2023 Jan;201(1):121-128. doi: 10.1007/s12011-022-03162-1. Epub 2022 Feb 19. PMID: 35184264.
4 Pickering G, Mazur A, Trousselard M, Bienkowski P, Yaltsewa N, Amessou M, Noah L, Pouteau E. Magnesium Status and Stress: The Vicious Circle Concept Revisited. Nutrients. 2020 Nov 28;12(12):3672. doi: 10.3390/nu12123672. PMID: 33260549; PMCID: PMC7761127.
5 Gröber U, Werner T, Vormann J, Kisters K. Myth or Reality-Transdermal Magnesium? Nutrients. 2017 Jul 28;9(8):813. doi: 10.3390/nu9080813. PMID: 28788060; PMCID: PMC5579607.
6 Dalia AA, Essandoh M, Cronin B, Hussain N, Gerstein NS, Schulman P. A Narrative Review for Anesthesiologists of the 2017 American Heart Association/American College of Cardiology/Heart Rhythm Society Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death. J Cardiothorac Vasc Anesth. 2019 Jun;33(6):1722-1730. doi: 10.1053/j.jvca.2019.01.004. Epub 2019 Jan 4. PMID: 30685157.

© Copyright 2025 Personalabs. All Rights Reserved.