- Fast results
- 4,000+ locations
- 4.8 star rating
Need Help? (888) GET LABS


The Mean Corpuscular Hemoglobin Concentration (MCHC) is a routine component of a complete blood count (CBC), aiding healthcare providers in diagnosing various conditions. While MCHC values offer valuable insights into blood health, they must be considered alongside other CBC results for accurate interpretation. Still, knowing what high and low MCHC results mean provides you clarity on your blood health. Read on to find out more about this test.
The Mean Corpuscular Hemoglobin Concentration (MCHC) blood test measures the average concentration of hemoglobin within your red blood cells (RBCs). It reveals how much hemoglobin (the oxygen-carrying protein) is packed into each cell relative to its size. Deviations from the normal MCHC range can indicate various conditions, such as certain types of anemia.
The MCHC blood test is included in a complete blood count (CBC). Hence, it can be taken as part of a routine exam. However, it can also serve as a valuable diagnostic tool for detecting diseases such as certain types of anemia, liver disease, inflammation, and some blood disorders.
RBCs or erythrocytes make up 40% of the blood(1) and facilitate oxygen distribution in tissues. With hemoglobin playing a crucial role in this function, understanding their concentration reveals abnormalities that impede cellular respiration.
However, the MCHC blood test may not suffice for your doctor to diagnose certain conditions accurately. Other tests, some of which are already included in the CBC, will be performed depending on your symptoms.
Also Read: 5 Ways to Fix Low Red Blood Cell (RBC) Count
You must provide a blood sample during the MCHC blood test. A licensed medical technician will draw the blood, usually from your vein, and analyze the sample. Specifically, the average amount of hemoglobin in the RBCs and the blood volume will be calculated.
For CBC, you don’t need to fast or do special preparations. Still, consult your healthcare provider for specific instructions before the test. This way, you can ensure accurate results.
Also Read: Preparing for a Blood Test: Things You Should Do to Get the Most Accurate Results
The CBC blood test result will indicate your MCHC and the reference value interval. Typically, a healthy adult’s MCHC falls within the range of 31.5 to 35.7 g/dL. It may vary depending on the lab performing the test. If your test results go outside the normal range, it could be due to specific causes, which are discussed below.
You have deficient MCHC if the value falls below 31.5 g/dL. Although it acts as a sign and not a definitive indicator, low MCHC can be associated with the following disorders.
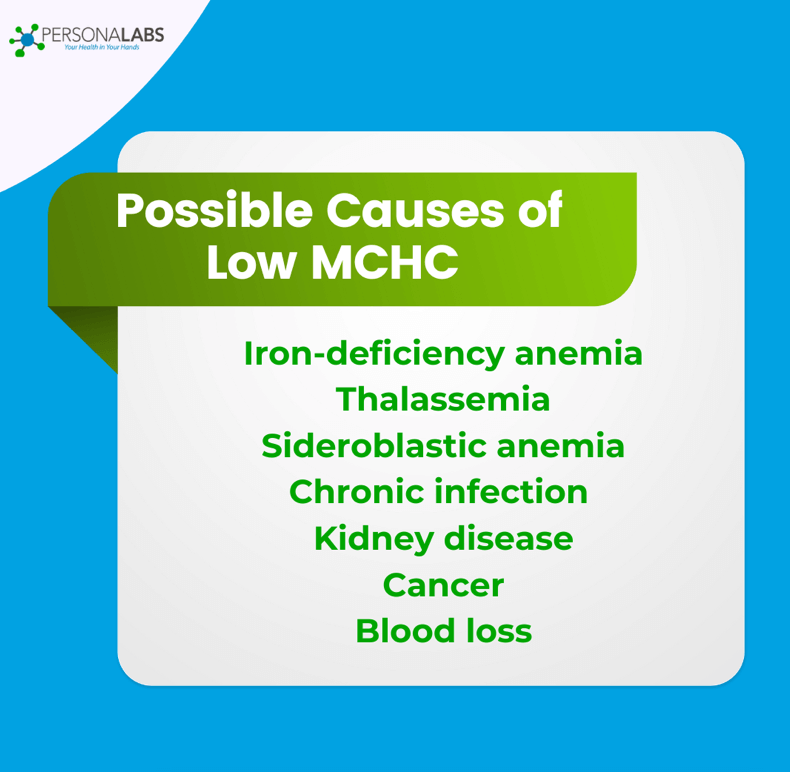
Iron-deficiency anemia disrupts the production of hemoglobin(2), the protein within red blood cells responsible for carrying oxygen. Because iron is a vital component of hemoglobin, a deficiency leads to red blood cells containing less hemoglobin than normal.
This decreased hemoglobin content within each cell results in a lower MCHC, as the average hemoglobin concentration within a given volume of red blood cells is reduced. Essentially, the red blood cells are smaller and paler due to insufficient hemoglobin.
Low MCHC is also linked to Thalassemia, which is a group of hereditary blood disorders that cause diminished hemoglobin production. Specifically, it leads to a reduced synthesis of either the alpha or beta globin chains(3) that make up hemoglobin. This impaired production results in red blood cells that are smaller than normal (microcytic) and contain less hemoglobin than they should (hypochromic).
Consequently, the concentration of hemoglobin within these cells, reflected by the MCHC value, is lower than the typical range.
Sideroblastic anemia(4) disrupts the typical production of hemoglobin within red blood cells. Specifically, the body struggles to incorporate iron into heme, a crucial component of hemoglobin. This iron accumulation, often seen as sideroblasts in bone marrow, hinders the proper formation of functional hemoglobin molecules.
Long-term infections(5) can impact RBC production, primarily through the development of anemia of chronic disease, also known as anemia of inflammation. During prolonged infections, the body’s inflammatory response triggers the release of certain cytokines, which interfere with iron metabolism. As a result, it hinders the body’s ability to utilize iron for hemoglobin production, impacting the maturation of red blood cells.
Kidney disease often leads to a decreased production of erythropoietin(6), a hormone vital for stimulating red blood cell production in the bone marrow. Individuals with kidney disease may experience anemia, characterized by fewer red blood cells. This reduced red blood cell count, coupled with poor iron utilization, can result in the production of red blood cells with lower hemoglobin concentrations. Since MCHC measures the average concentration of hemoglobin within red blood cells, this deficiency in hemoglobin per cell manifests as a lower MCHC value in blood tests.
Cancer, particularly certain types like leukemia, kidney cancer(7), or those that metastasize to the bone marrow, can disrupt normal red blood cell production, leading to a decreased MCHC. This occurs as cancerous cells infiltrate the bone marrow, hindering the development of healthy red blood cells capable of carrying adequate hemoglobin.
Chemotherapy and radiation treatments, often used to combat cancer, can also damage bone marrow(8) and further suppress red blood cell production, contributing to a lower MCHC. Additionally, chronic inflammation associated with some cancers can interfere with iron utilization, a vital component of hemoglobin, indirectly causing a reduction in MCHC levels.
A low MCHC blood test result can also be due to blood loss or a recent blood transfusion since hemoglobin is likely diluted for a short period. Simply put, any condition that interferes with RBC production can cause low MCHC. Hence, treating the underlying health problem should help improve hemoglobin concentration.
Did You Know? Vitamin B12 deficiency can result in larger red blood cells, as indicated by a high mean corpuscular volume (MCV) test result, ultimately leading to low MCHC. You can learn if you lack this vitamin by knowing the symptoms and taking the vitamin B12 blood test.
Elevated MCHC occurs when your test result exceeds 35.7 g/dL. While not necessarily a diagnosis, a higher-than-normal hemoglobin concentration can be found in the following conditions.
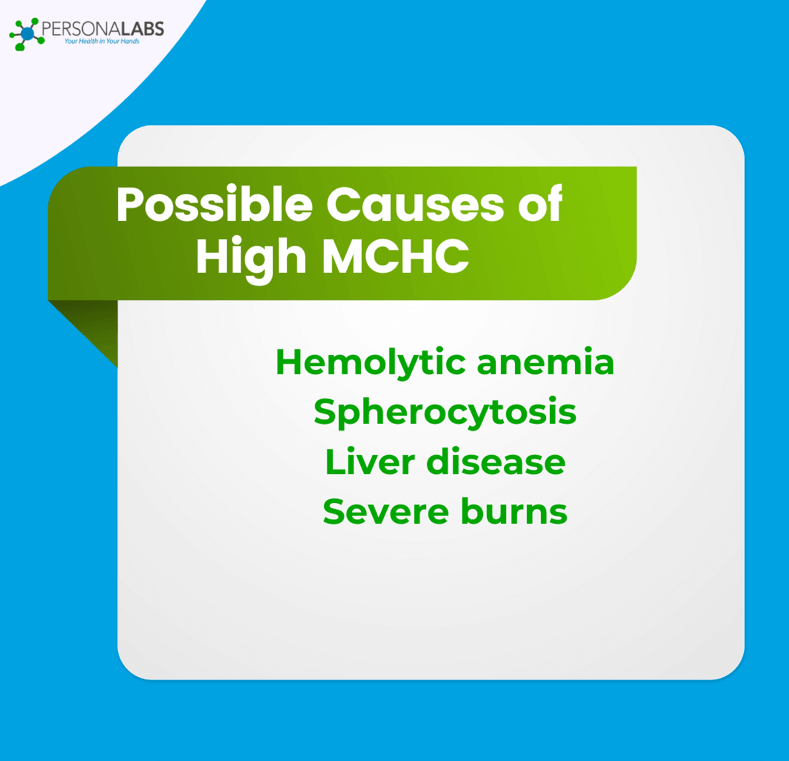
You may get a high MCHC blood test result when your RBCs are destroyed (hemolysis) faster than they are produced—which is essentially hemolytic anemia. Hemolytic anemia(9), particularly autoimmune hemolytic anemia (AIHA), can lead to an elevated MCHC due to the destruction of red blood cells.
When the immune system attacks and damages these cells, some may rupture, releasing their contents. However, others may shrink or become spherocytic, meaning they take on a spherical shape. This shape change concentrates the hemoglobin within the remaining red blood cells, resulting in a higher ratio of hemoglobin to red blood cell volume.
Red blood cells are disc-shaped. But if you have spherocytosis, a genetic blood disorder, your RBCs look spherical, making them more breakable, which generates high MCHC(10). These spherical cells have a reduced surface area relative to their volume, leading to cellular dehydration.
As water is lost from the cell, the concentration of hemoglobin within the remaining red blood cell volume increases. This higher concentration of hemoglobin within each cell results in an elevated MCHC on a CBC test.
Liver disease itself doesn’t directly cause a true elevation of MCHC. However, certain complications of liver disease(11) can indirectly influence MCHC readings, often through mechanisms that affect red blood cell integrity.
For instance, severe liver dysfunction can lead to abnormalities in red blood cell membranes, making them more fragile or prone to clumping. This fragility can result in red blood cell destruction, and the remaining cells may appear to have a higher concentration of hemoglobin.
Severe burns(12) can lead to a high MCHC due to a complex interplay of factors affecting red blood cells and blood volume. The intense heat from burns damages red blood cells, causing them to shrink and become more concentrated.
Additionally, fluid loss from the burn site leads to hemoconcentration, where the remaining blood volume has a higher concentration of red blood cells, thus increasing the hemoglobin concentration within those cells. The combination of these effects results in a higher MCHC value observed in a complete blood count.
Other conditions can also indirectly contribute to elevated MCHC, like hyperthyroidism and dehydration. Nonetheless, treatment for high MCHC is specific to the underlying cause.
Pro tip: The CBC is a standard test to evaluate blood health and other common health problems. As it comes in a package, a diagnosis based on the CBC should not be based on single tests. For example, if your MCHC is below the normal range, check if you also have low MCH and MCV.
MCH stands for mean corpuscular hemoglobin. It measures the average amount of hemoglobin within each red blood cell, expressed in picograms. MCH is different from MCHC (mean corpuscular hemoglobin concentration) in that it measures hemoglobin mass in a single red blood cell (RBC). MCHC, on the other hand, measures the average concentration of hemoglobin within a given volume of packed red blood cells, expressed as grams per deciliter.
Certain cancers impact hemoglobin development or destruction, which in turn causes low MCHC. For example, cancers that interfere with bone marrow activities, such as leukemia, multiple myeloma, and lymphoma, prevent RBC production. Likewise, cancers that cause bleeding, including colon and stomach cancer, lead to the same effect.
Yes, dehydration can elevate your MCHC. When dehydrated, blood plasma volume is reduced, making the blood more concentrated. RBC numbers remain the same, but the density of hemoglobin can increase.
As MCHC is included in the CBC, you can book the test as part of your routine wellness checkup. However, healthcare providers typically underscore MCHC results together with other tests, like MCH and MCV, when diagnosing certain blood disorders, like anemia. To better understand what your MCHC blood test result says about your health, consult your doctor and note any unusual conditions or symptoms you experience.
1 Sharma R, Sharma S. Physiology, Blood Volume. 2023 Apr 10. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 30252333.
2 Leung AKC, Lam JM, Wong AHC, Hon KL, Li X. Iron Deficiency Anemia: An Updated Review. Curr Pediatr Rev. 2024;20(3):339-356. doi: 10.2174/1573396320666230727102042. PMID: 37497686.
3 Motiani A, Zubair M, Sonagra AD. Laboratory Evaluation of Alpha Thalassemia. [Updated 2024 Feb 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK587402/
4 Ashorobi D, Kaur A, Chhabra A. Sideroblastic Anemia. [Updated 2024 Dec 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538287/
5 Viana MB. Anemia and infection: a complex relationship. Rev Bras Hematol Hemoter. 2011;33(2):90-2. doi: 10.5581/1516-8484.20110024. PMID: 23284251; PMCID: PMC3520628.
6 Li D, Zhang Q, Ruan Z, Zhang Y, Liu X, Zhang G, Zhao H, Li J, Wu B. The relationship between mean corpuscular hemoglobin concentration and mortality in hypertensive individuals: A population-based cohort study. PLoS One. 2024 May 9;19(5):e0301903. doi: 10.1371/journal.pone.0301903. PMID: 38722884; PMCID: PMC11081350.
7 He Q, Wei C, Cao L, Zhang P, Zhuang W, Cai F. Blood cell indices and inflammation-related markers with kidney cancer risk: a large-population prospective analysis in UK Biobank. Front Oncol. 2024 May 23;14:1366449. doi: 10.3389/fonc.2024.1366449. PMID: 38846978; PMCID: PMC11153768.
8 Crawford J, Herndon D, Gmitter K, Weiss J. The impact of myelosuppression on quality of life of patients treated with chemotherapy. Future Oncol. 2024;20(21):1515-1530. doi: 10.2217/fon-2023-0513. Epub 2024 Apr 8. PMID: 38587388; PMCID: PMC11441072.
9 Baldwin C, Pandey J, Olarewaju O. Hemolytic Anemia. 2023 Jul 24. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. PMID: 32644330.
10 Häuser F, Rossmann H, Adenaeuer A, Shrestha A, Marandiuc D, Paret C, Faber J, Lackner KJ, Lämmle B, Beck O. Hereditary Spherocytosis: Can Next-Generation Sequencing of the Five Most Frequently Affected Genes Replace Time-Consuming Functional Investigations? Int J Mol Sci. 2023 Nov 30;24(23):17021. doi: 10.3390/ijms242317021. PMID: 38069343; PMCID: PMC10707146.
11 Parsarad, M., Ehtiati, S., Olazadeh, K., Dehghan, S. F., Ghorbani, M., Azimian, A., & Vaziri, M. H. (2025). Hematological biochemical and liver function changes associated with BTEX exposure in a six year retrospective cohort study. Scientific Reports, 15(1), 1-13. https://doi.org/10.1038/s41598-025-89757-9
12 Kiani Z, Khorsand N, Beigi F, Askari G, Sharma M, Bagherniya M. Coenzyme Q10 supplementation in burn patients: a double-blind placebo-controlled randomized clinical trial. Trials. 2024 Mar 2;25(1):160. doi: 10.1186/s13063-024-08006-y. PMID: 38431600; PMCID: PMC10908042.

© Copyright 2025 Personalabs. All Rights Reserved.